The role of vitamin D and the treatment of vitamin D deficiency
Click on the appropriate heading below to view full information
The role of vitamin D
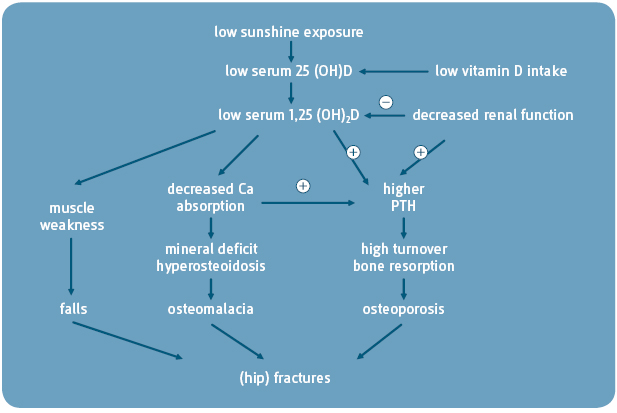
 Vitamin D through its active form (1,25-dihydroxyvitamin D) is essential for intestinal Ca absorption and plays a central role in maintaining Ca homeostasis and skeletal integrity1
Vitamin D through its active form (1,25-dihydroxyvitamin D) is essential for intestinal Ca absorption and plays a central role in maintaining Ca homeostasis and skeletal integrity1
In vitamin D deficiency there is a decrease in the concentration of 25(OH) vitamin D (25-hydroxy vitamin D) and an increase of varying degrees in the parathyroid hormone (PTH) level2
The increased serum PTH stimulates bone turnover, leading to bone loss3
In periods of protracted vitamin D deficiency, bone loss is increased and this may lead to osteoporosis3
Vitamin D deficiency
“There is widespread acknowledgement of the presence of vitamin D deficiency in the community and the pressing need to address this deficiency1“
Prof Kevin Cashman, UCC, commenting on the results of the Irish NANS Study 2013.
- The North American Institute of Medicine (IOM)’s DRI Committee for Ca and vitamin D proposes a serum 25(OH)D concentration of 50nmol/L that would meet the needs of 97.5% of normal healthy persons1
- In agreement with the Scientific Advisory Committee on Nutrition (SACN)2 report, the Royal Osteoporosis Society (ROS)3 in the UK proposes vitamin D thresholds as follows:Plasma 25 (OH) D < 25 nmol/L is deficientPlasma 25 (OH) D of 25 – 50 nmol/L may be inadequate in some peoplePlasma 25 (OH) D > 50 nmol/L is sufficient for almost the whole population
- The Endocrine Society Clinical Practice Guideline defines vitamin D deficiency as 25(OH)D below 50nmol/L and vitamin D insufficiency below the range of 52.5-72.5nmol/L4
- The American Geriatrics Society Consensus Statement on Vitamin D for the Prevention of Falls and their Consequences recommends that a serum 25(OH)D concentration of 75nmol/L should be a minimum goal to achieve in older adults, particularly in frail adults who are at greater risk of falls, injuries and fractures5
- The guideline statement from the Scientific Advisory Council of Osteoporosis Canada states that the optimal serum 25-hydroxyvitamin D (25OHD) level for bone health is uncertain, however ≥50 nmol/L is generally considered adequate for bone and overall health in healthy individuals.6
- The American Academy of Paediatrics (AAP) states that serum concentrations of 25(OH)D in infants and children should be at least 50nmol/L7 The Canadian Paediatric Society defines deficiency as serum 25(OH)D levels <25 nmol/l, insufficiency as 25-75nmol/L but highlights a range of 75-225nmol/L as optimal for parathyroid hormone production, minimisation of resorption from bone and stabilisation of intestinal calcium absorption8
- The Evidence-Based Recommendations from the Cystic Fibrosis Foundation, published in JCEM 2012, recommend a minimum serum 25(OH)D level of 75nmol/L for people with cystic fibrosis9
Clinical features of vitamin D deficiency
Osteomalacia and vitamin D deficiency treatment
- In young children, who have little mineral in their skeleton, vitamin D deficiency results in a variety of skeletal deformities classically known as rickets5
- In adults, the epiphyseal plates are closed and there is enough mineral in the skeleton to prevent skeletal deformities so that this mineralisation defect, known as osteomalacia, often goes undetected5
- However osteomalacia causes a decrease in Bone Mineral Density (BMD) and is associated with isolated or generalised aches and pains in bones and muscles5
Osteomalacia is softening or weakening of the bones due to a lack of vitamin D or due to a problem with the body’s ability to break down and absorb vitamin D.
- Vitamin D deficiency causes muscle weakness
- Affected children have difficulty standing and walking
- The elderly have increasing sway and more frequent falls, thereby increasing their risk of fracture5
The pathophysiologic pathways from vitamin D deficiency to osteoporosis, osteomalacia, falls and fractures:3